Infant fever is a very significant concern for many parents. As a family doctor, it is a common problem that is part of my daily life. I regularly answer multiple questions from parents who want to be reassured.
Does their toddler have a high fever? How and why should parents lower their baby’s fever? Can fever be dangerous?
See below for answers to the most frequently asked questions. They provide an overview of the situation to better understand and manage fever in your toddlers.
Infant Fever: What you need to know? is it bad for Baby’s health?
Infant Fever is not a disease, but rather a sign of a disease. Most of the time, fever indicates that your child’s body is fighting a viral or bacterial infection.
The internal temperature of her body increases voluntarily in order to fight the virus or bacteria. In addition, raising the temperature would activate your child’s immune system.
Baby Fever is therefore a natural ally that testifies to the effectiveness of the body’s defense mechanisms, rather than an enemy to be fought.
The degree of fever is not related to the severity of the disease. For example, a high fever may accompany a common cold, while a child with meningitis may have a much lower fever.
It is the general condition of a child with a fever that matters most. A baby with a mild fever, but who is drowsy or irritable, is more worrying than a child with a high fever, but who maintains a good general condition.
Fever is a normal reaction of the body to help it fight off an infection most often. It is important to know how to measure it. In itself, fever is most often mild and requires treatment only when it exceeds 38.5°C and is poorly tolerated.
Infant Fever: What is the normal baby temperature?
The normal baby temperature (measured in the mouth) is approximately 37°C (98°F). The temperature rectal (measured in the rectum) is approximately 0.5°C higher than that taken by the mouth.
Rectally, the normal temperature is about 37.5°C (99.5°F). The temperature can vary during the day, even in the case of healthy children.
Many doctors talk about fever temp when the temperature exceeds 37.5°C (99.5°F) by mouth or 38.0°C (100.4°F) through the rectum or when the temperature axillary (measured under the armpit) exceeds 37.2°C (99°F) (the temperature measured in the ear is not accurate in children under 6 months of age and is often not recommended for children under one or two years of age)
Fever is primarily a physiological defense mechanism against infectious diseases that has beneficial effects in fighting infections, reducing the multiplication of viruses and bacteria and increasing the ability of white blood cells to respond to infection.
It is the witness of the activation of the immune defense against an infectious agent. In principle, we should not fight against our defense mechanisms, but only against their excesses and inconveniences.
If your child has a fever of 40°C, this does not necessarily mean that his illness is serious… The importance of fever has no direct correlation with the severity of the disease. However, when the fever is high, there is a greater chance that the infection is of bacterial origin.
What are Infant fever symptoms?
- vomits a lot;
- seems dehydrated;
Call 911 if you believe that the urgency and seriousness of the situation require ambulance transportation.
- does not react much to his environment;
- a pale or poorly colored complexion;
- is difficult to wake up, has persistent drowsiness and irritability;
- has unusual redness;
- complains of a severe headache, pain, or stiffness in the neck;
- bluish skin rashes, which look like bruises;
- seizure attack: he loses consciousness for a short time;
- he moves his limbs in a jerky manner and has repulsed eyes;
- suffers from breathing difficulties.
Some Causes of Fever
Infant Temperature is not necessarily proportional to the severity of the infection. For example, Baby temperature can be linked to a pushed dental or vaccine. It is also possible that baby will suffer from a bacterium-related infection, in which case it will be necessary to prescribe antibiotics.
As a general rule, it is recommended that a physician be consulted in the following cases:
- as soon as the fever appears if the infant is less than six months old;
- baby has a chronic disease;
- infant cannot tolerate the treatment, if the temperature does not drop for 2 days or if he vomits, remains amorphous, or seems not to breathe normally;
- if the fever exceeds 40.5°C;
- in case of convulsion: if the fever does not go down or increases very quickly, there is a risk of convulsion (stiffness of the limbs, tremors).
- While a short-term seizure (less than two minutes) does not cause any particular pain, it is very impressive for the parents. If it lasts more than 5 minutes or is accompanied by a loss of consciousness, it is essential to immediately contact 911 or ( emergency number).
When should I try to reduce my baby’s temperature?

In older children, fevers are more common in older children. worrying as well as dangerous. They mean usually that the body is fighting an infection.
We’ll treat the child to make him feel better. If it is irritable or suffering, you may want to give it to him/her a drug to lower the fever.
A fever between 38°C and 40°C is usually caused by viruses and lasts no more than two days. If the child is between 3 months and 4 years old and has a low fever high (up to 37.8°C[100.2°F]), it is not necessary to give him some medicine.
If he’s irritable and if the temperature exceeds 37.8°C (100.2°F), you can treat it with a drug. If your infant is less than 3 months old and has a rectal temperature of 100.4°F (38°C) or higher, call your doctor or go to the emergency room immediately. The fever may be a sign of a serious infection in young babies.
What type and dose of medication are needed to lower the fever?
Acetaminophen (Tylenol, Tempra, Panadol) and ibuprofen (Advil and Motrin) are drugs that relieve pain and lower fever. In the case of infants (less than 6 months), ibuprofen can give no more side effects.
The amount of medication a child needs is a function of his weight and age. If age and table weights do not match, use the weight to help you determine the amount of acetaminophen or ibuprofen to be given.
These doses may be higher than those indicated on the drug container. If you’re not sure how much to give, consult your family doctor for advice.
Suggestions on how to administer the drug :
- – Do not give more than 5 doses per day.
- – Do not give medication to an infant with less than four months, unless your family doctor recommended it to you.
- – Read the labels carefully. Make sure to give the right dose of medication. There are several forms of acetaminophen: drops, oral solutions, chewable tablets, and caplets. Each shape has a different strength.
- – Do not replace the drops with elixir because the drops are stronger.
- – When giving drops, fill in the dropper to the line.
- – To give the drinkable solution, use the container to measure to ensure you give the right dose. One teaspoon won’t give you a precise dose.
You can also get a container to be measured at the pharmacy or ask your pharmacist.
Are there other ways to relieve my child?
Yes. To control fever, you can:
- Give a lot of fluids to the child to prevent dehydration (lack of fluid in the body) and help control body temperature. Water, broths, ice cream, and aromatized gelatin are good choices. Even if your child does not absorb enough liquids, don’t force him to eat if he doesn’t want to.
- Promote rest. Moving can increase body temperature.
- Adjust the room temperature between 21 ° C (70 ° F) and 23 ° C (74 ° F).
- Dress lightly (e. g. light cotton pajamas) so that body heat can escape. Do not cover the child too much to avoid imprisoning body temperature and thereby increasing it.
- If the child shuts, add a cover; Remove it when it stops spawning.

When should I call the doctor?
In a child, rely more on his or her behavior only at the temperature indicated on the thermometer. Read the following tips to decide when to call your doctor. If you think your child needs help or if you have any questions, he/she is important to call your doctor.
– For infants under one month of age. Call immediately your family doctor if your baby’s temperature measured orally is more than 38.0°C (100.4°F) or more than 38.5°C (101.3°F) measured rectally, even if it has not been looking sick.
Your doctor may want to see him and even hospitalize him to find the cause of the fever. Babies, at this age, can quickly become very sick. Also call your doctor if the child has any of the following signs, even in the absence of fever.
– Between 1 and 3 months. Call the doctor if your baby has a fever of 38.5°C (101.4°F), even if the child does not have sick air or a fever of 38°C (100.4°F) that lasts for more than 24 hours. Also, call him if
your baby has one of the following signs.
– Between 3 months and 2 years. If your child has a fever of At 38.6°C (101.4°F), monitor his behavior. Call the doctor if the fever increases, if it has been going on for more than three days or if your child has one of the signs below. If the fever is 39°C (103°F), call your doctor even if the child looks fine.
– Children 2 years old and over. If your child has a fever of
At 38.6°C (101.4°F), monitor his behavior. Call the doctor if the fever increases, if it has been going on for more than three days or if your child has one of the following signs below.
Call your doctor if your child has one of the following signs:
- – Behavioural changes
- – Severe headaches
- – Vomiting or diarrhea on a constant basis
- – Rashes of skin
- – Dry mouth
- – Persistent sore throat
- – Persistent earache or if the child pulls his or her ear
- – Neck stiffness
- – Persistent fever for several days
- – Stomach ache
- – Acute crying
- – Fontanelle bulge (soft space on the head)
- – Irritability
- – Inactive or soft
- – Lack of appetite
- – Wheezing or difficulty breathing
- – Pale
- – Whining
- – Convulsions
- – Painful or swollen joints
What about immunization?
Immunization is your best prevention. The H. vaccine. Influenza has contributed to a decrease in severe bacterial infections in young people and children. The pneumococcal vaccine is now available for young children and helps to reduce the increase the risk of serious bacterial infections
in these children.
Fever Temperature Chart
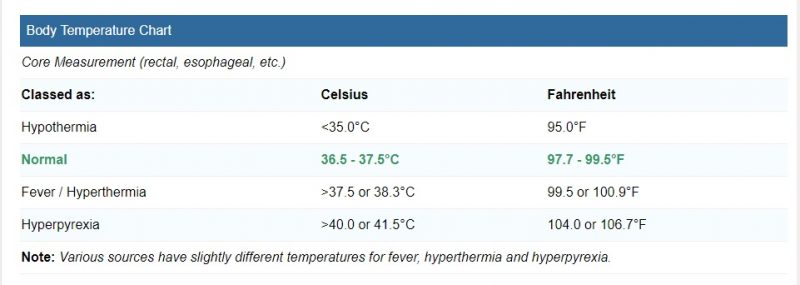
Fever Temperature Conversion Chart
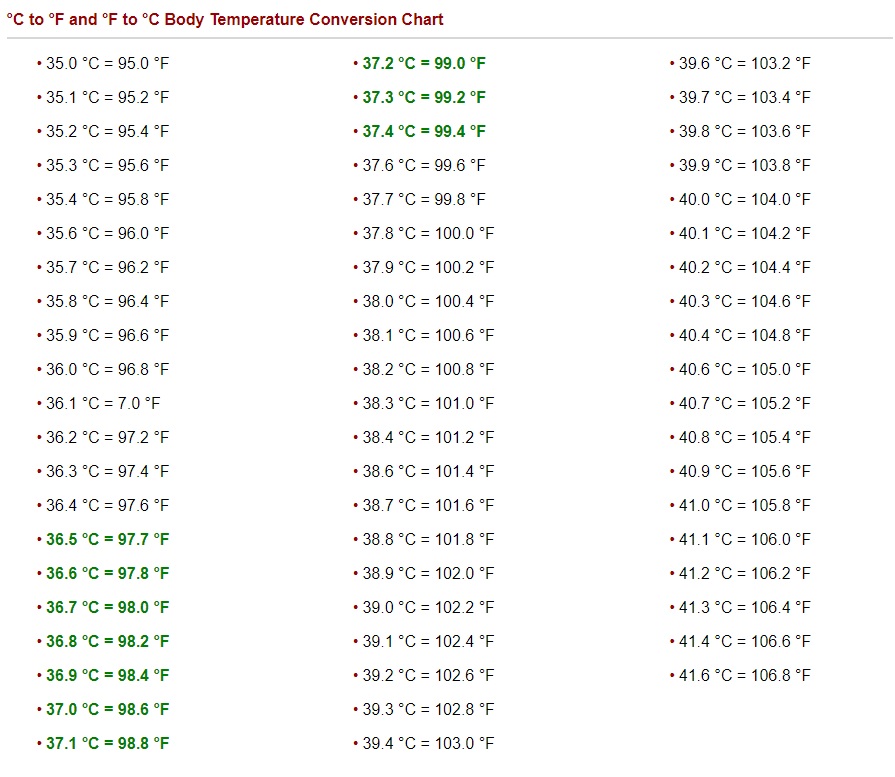
Your child’s temperature may vary depending on the method used. Rectally, the temperature is generally higher than orally. Similarly, the baby’s temperature taken by the mouth will be higher than that taken under the armpit. Your child has a fever if his temperature is equal to or higher than:
Baby Temperature Chart
| Normal temperature range |
|---|
| Body | Celsius (°C) | Fahrenheit (°F) |
|---|---|---|
| Oral | 35.5–37.5 | 95.9–99.5 |
| Rectal | 36.6–38 | 97.9–100.4 |
| Armpit | 34.7–37.3 | 94.5–99.1 |
| Ear | 35.8–38 | 96.4–100.4 |
How to test Infant Fever?
- 38.1°C (100.6°F) rectally for a child under 3 months ;
- 38.5°C (101.3°F) rectally for a child over 3 months
- 38.0°C (100.4°F) by mouth;
- 37.5°C (99.5°F) by axillary route (armpit).
Since the temperature obtained by the axillary route is less accurate, confirm it by a rectal route if:
- it exceeds 37.3°C (99.1°F); your child is hot and looks sick, even if it is below 37.3°C (99.1°F).
- To take your child’s temperature, use a digital thermometer. In addition to being safe, this type of thermometer allows you to take the temperature by rectal, oral, and axillary means.
- For hygienic reasons, reserve a thermometer for rectal use. Do not use a mercury thermometer because of the risk of toxicity if it breaks.




